Earlier this month, the Centers for Medicare & Medicaid Services (CMS) released its final rule on the Medicare Access and CHIP Reauthorization Act (MACRA), and efforts are well under way around the country to encourage a shift to value based payment models for Medicare providers. Meanwhile, the Medicare Payment Advisory Commission (MedPAC) recently recommended a move away from a key component of MACRA, the Merit-based Incentive Payment System (MIPS), toward a different approach to value-based payment. The goal of this briefing is to provide an update on MACRA implementation, the issues on the table as policymakers consider next steps around shifting the way providers are paid, and what this all means for improving health outcomes and quality.
Panelists:
Mark Miller, Medicare Payment Advisory Commission (MedPAC)
Elizabeth Mitchell, Network for Regional Healthcare Improvement
Aucha Prachanronarong, Division of Electronic and Clinician Quality, Centers for Medicare and Medicaid Services
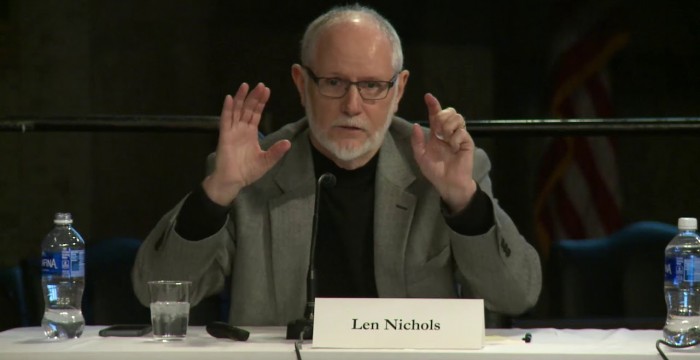
Len Nichols, George Mason University Center for Health Policy Research
Greg Woods, Division of Alternative Payment Model Infrastructure, Center for Medicare and Medicaid Innovation
Sarah Dash, Alliance for Health Policy (moderator)